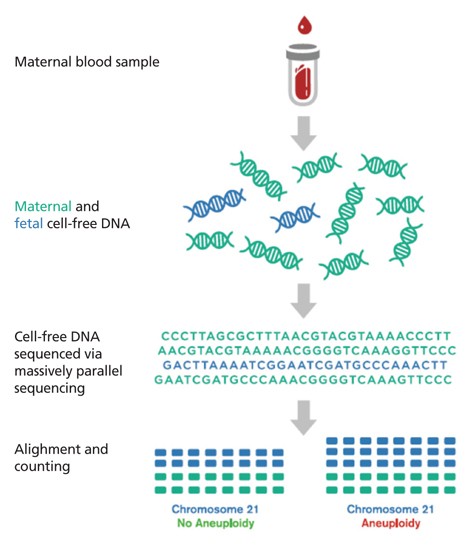
This recently developed test is performed from a peripheral blood sample of the pregnant woman after the 10th week of pregnancy and involves the non-invasive risk assessment (screening) for common chromosomal aneuploidies (Non Invasive Prenatal Testing-NIPT), using cell-free fetal DNA in maternal blood (plasma). Its accuracy is estimated at ~ 99% for the detection of Down syndrome (trisomy 21) and is relatively less accurate for other common chromosomal aneuploidies (e.g. 13, 18, X and Y).
Couples should be informed about all the available options in prenatal chromosomal testing, including non-invasive prenatal diagnosis (NIPT), which avoids the risk of invasive procedures, making, but:
- is not a diagnostic test and
- is currently limited to the risk assessment for only a few common aneuploidies, basically for Down syndrome
Therefore, the choice of performing NIPT should be a conscious choice of the couple, following appropriate genetic counseling, which should also provide information regarding the serious limitations of the test.
In conclusion, the advantages of NIPT, typically performed between the 10th and 20th week of gestation, focus primary on the ability to detect, with a relatively high success rate, embryos harboring classic aneuploidies-trisomies (for chromosomes 21, 18 and 13 and to a lesser extent for the sex chromosomes X and Y), without the (low) risk of pregnancy complications associated with invasive testing.
The indications for non-invasive prenatal diagnosis, now mainly focus on ‘medium’ risk pregnancies, as revealed through previous first trimester ultrasound (NT) combined with biochemical markers and maternal age.
The limitations of NIPT, as currently applied internationally by all laboratories and according to internationally accepted guidelines, include: