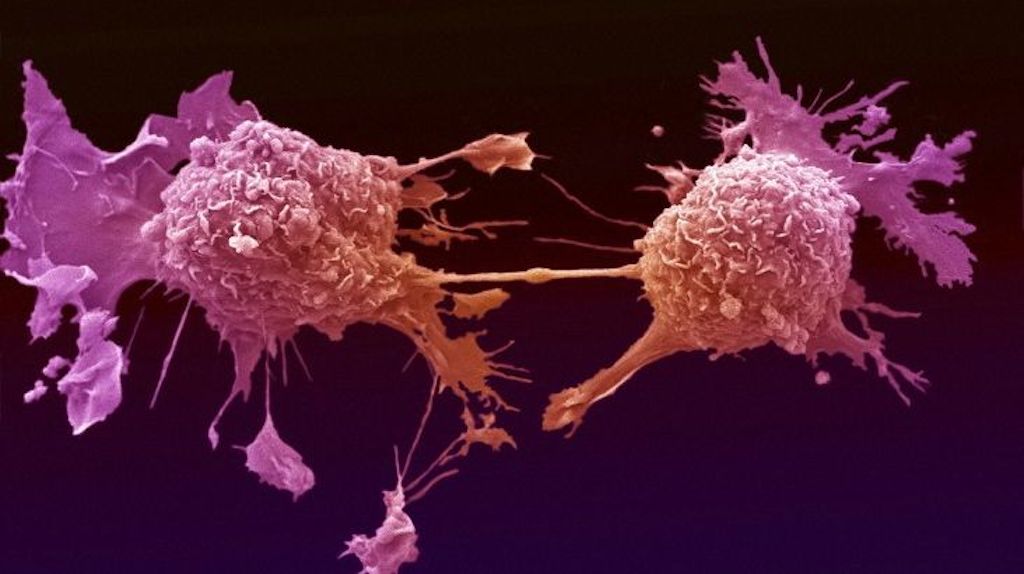
Cancer is a very heterogeneous disease, resulting from accumulation of mutations in the DNA. The etiology of cancer is multifactorial, involving genetic, environmental and other medical factors as well as lifestyle factors that interact to develop a specific malignancy.
About 5% -10% of cancers are hereditary and genetic testing has been used for certain hereditary forms of cancer for more than a decade. The knowledge of the genetics of cancer improves rapidly with the understanding of the molecular mechanisms, which help to identify individuals at high risk, enables characterization of the disease, allows for customized treatments adapted to the molecular basis of the disease, and leading to the development of new therapies. This expansion of knowledge has implications for all aspects of cancer management, including prevention, detection and treatment.
Genetic information provides a valuable tool for identifying individuals at increased risk of cancer. The sources of genetic information include genetic analysis of DNA from biological samples, information from family history of the individual patient as well as the findings from the physical examination and medical history. The information from the analysis of DNA can be collected, stored and evaluated at any time during a person’s life, from birth to after death. The family history may also identify individuals with moderate to increased cancer risk or can serve as the first step to identify a hereditary predisposition which confers a very high risk of cancer.
For a significant number of cancers, genetic testing can now be used to identify a specific mutation associated with hereditary risk and in turn to determine whether other members of the family have inherited the mutation associated with the disease.It should be noted that the percentage of people carrying a specific mutation and who will develop the disease is referred to as penetrance. Generally, common genetic variants-mutations associated with predisposition to cancer, have a lower penetrance compared to rare pathological genetic mutations.
The proper identification of individuals and families, who are at increased risk of developing cancer, is an important objective of primary care. Once identified, these individuals can then be evaluated more closely, through appropriate genetic counseling, in relation to the risks and the required genetic test that will lead to the implementation of a custom-tailored disease management.
A wide range of genomic aberrations, including point mutations, copy number changes and chromosome abnormalities may lead to the development of cancer. Most of these genetic lesions are somatic, meaning that they are present only in tumor cells and not in the gametes of a patient, and therefore are not related to hereditary cancers. To date, approximately 85 different genes have been identified with germline mutations and more than 300 genes with somatic mutations, which have been shown to be involved in human cancers. Until now, the most widely used method for the genetic testing of hereditary cancers is the analysis by Sanger DNA sequencing, which is considered the ‘golden standard’ for detecting mutations. Nevertheless, because the genes associated with hereditary forms of cancer are very large and there are no specific mutation hot spots, this traditional method has generally proven to be time consuming, costly and with a moderate to low diagnostic yield.